Treatment Options for Metatarsalgia
-
Home

-
Orthopaedic Specialties & Services

-
Treatments

- Treatment Options for Metatarsalgia
Metatarsalgia (metatars = metetarsal, algia = pain) is a condition in which one experiences pain and inflammation along the metatarsal head at the ball of the foot. It can be caused by a wide variety of conditions including trauma, ill-fitting shoe wear, excessive exercise, and even some chronic conditions of the foot and ankle. For example, high heels that put increased pressure along the forefoot, as well as very hard, stiff shoes can cause metatarsalgia. Chronic conditions such as hammertoe deformity or cavorvarus foot deformity (high arches) can also put you at risk of developing metatarsalgia. Some patients may also develop metatarsalgia after having surgery to the foot and ankle due to a change in toe length, foot position, or gait mechanics. As we age, we also start to lose the fatty layer of tissue that cushions our distal footpad which can make weight bearing more painful. Lastly, this condition can be idiopathic, meaning there is no known cause.
Metatarsalgia is most common along the second toe. Typical symptoms that you may experience with metatarsalgia are pain and swelling along the bottom of the forefoot, worsened by weight bearing, and increased activity. The pain can be sharp and it may feel like you are walking on a marble, or like there is a rock in your shoe. You also may not tolerate walking barefoot or on hard surfaces very well. Many patients will compensate by avoiding pressure on the ball of their foot.
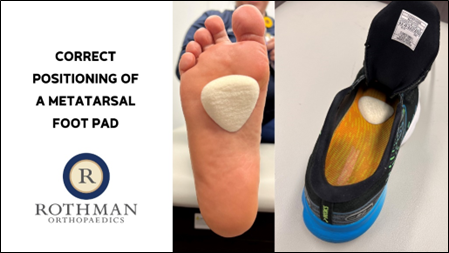
If you are experiencing metatarsalgia pain, there are some easy conservative modalities you can try to help alleviate your symptoms. First, try to reduce swelling by taking nonsteroidal anti-inflammatories and using a cool compress along the bottom of the foot for 15-20 minutes every 2-3 hours. A neat trick is freezing a plastic water bottle and gently rolling this along the bottom of your footpad. You can also try a compression stocking. Next, activity modification is very important. You should undergo a period of relative rest and limit all running, jumping, and high impact activities for at least 4-6 weeks. Keeping your step count to less than 4,000 per day or less than 50% of your daily routine is helpful. Additionally any activities in which you push off from the bottom of your forefoot should be avoided, such as calf raises or going up on your tiptoes. It is also very important you have good shoe wear that provides adequate support, such as a well-cushioned sneaker. A metatarsal pad can be placed inside the shoe, proximal to the metatarsal heads, to help offload the painful region of the foot and make weight bearing more comfortable, as well. Lastly, maintaining a healthy weight can help relieve pressure on the foot.
If you are still having pain after 3-4 months of trying the above lifestyle modifications, then it is important to seek assistance from an experienced foot and ankle physician. Injections are not typically recommended for the treatment of metatarsalgia, as they can cause tissue disruption and deformity to the toe. Be sure and speak to your foot and ankle physician before getting an injection to your foot. After an appropriate course of conservative management, surgery may be indicated. Surgical treatment typically involves an osteotomy, in which a cut is made through your metatarsal bone to shorten it, which relieves pressure along the joint. Any other toe deformity that you may have, such as a hammertoe, can also be corrected at that time. This procedure can often be performed through a minimally invasive approach, with small incisions and a quicker recovery. Typically, patients tolerate this procedure well and are weight bearing comfortably in a shoe around 6 weeks post-operative.




