Advanced Precision in Computer-Assisted Total Hip Replacement Surgery
Over 40 million older adults are projected to suffer from hip osteoarthritis by 2030 (1). Total hip replacement(THR) is a very effective surgery for the treatment of hip osteoarthritis. It is projected that 635,000 THRs will be performed annually by 2030 (2). Despite overwhelmingly excellent results, complications including instability, periprosthetic fracture, loosening, infection, and limb length discrepancy still occur. Instability (dislocation) is one of the most common reasons for reoperation after total hip arthroplasty. Placement of implants outside of the desired parameters, often called the “functional safe zone”, increases the risk of dislocation. Thus, stability of a hip replacement is enhanced by accurate positioning of components.
Computer-assisted surgery (CAS), or computer navigation, allows the surgeon to optimize implant positioning by creating a virtual 3-dimentional model based on specific anatomic landmarks. The main objective of CAS is to decrease the rate of reoperation by increasing stability. Secondary goals include determining ideal leg length, implant size, and offset. Several studies have shown that computer-assisted THR improves implant positioning compared to conventional THR. However, it is unclear whether computer or robotic assistance, although more accurate, provides any improvement in clinical outcome.
There are different types of computer-assisted platforms, robotic and non-robotic.
Both robotic and non-robotic systems work via specific steps in order to increase accuracy and precision. If a preoperative CT scan Is required, a digital 3-Dmodel of the patient’s anatomy is created from the image. Based on the model, optimal implant sizes and positioning are determined. Regardless of whether preoperative imaging is obtained, during surgery, specific pelvic and femoral landmarks are registered onto a virtual model. Finally, with or without robotic assistance, the hip is prepared and shaped to fit the components. The computer monitor displays specific measurements and angles for ideal implant positioning. Lastly, the final implants are impacted into place.
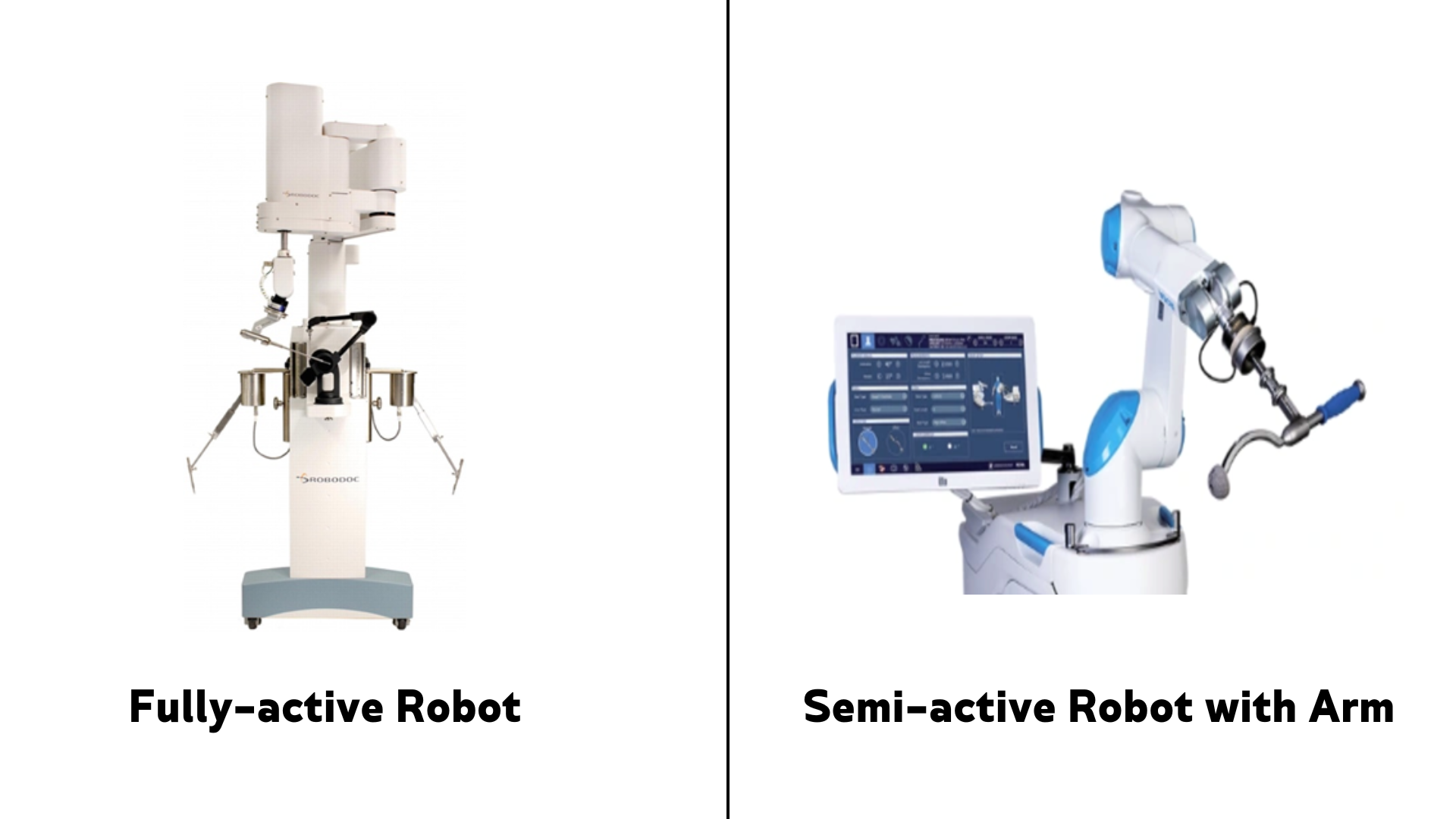
Computer-assistance in hip surgery was introduced in the 1990s. The first application of computer-assisted hip replacement surgery was the ROBODOC. The ROBODOC is considered a “fully active system”, meaning that it is autonomous. Specific information is required to be input preoperatively, then ROBODOC performs the procedure without direct surgeon control. Due to complications with these fully active robotic systems, often stemming from the lack of surgeon control, semi-active systems were developed. Semi-active robotic navigation allows the surgeon to maintain control of the operation while the robot provides tactile and auditory feedback for guidance. Modern robotic systems have adopted this concept, while active robots are not used in the United States. There are several semi-active robotic platforms. Although there are some differences, essentially all require the surgeon to place pins and/or screws into anatomic landmarks which provide registration into the software. Proper implant positioning is determined, then the robotic arm is used by the surgeon for bone preparation and implant positioning. The robotic arm will only move within specific boundaries to ensure accuracy.
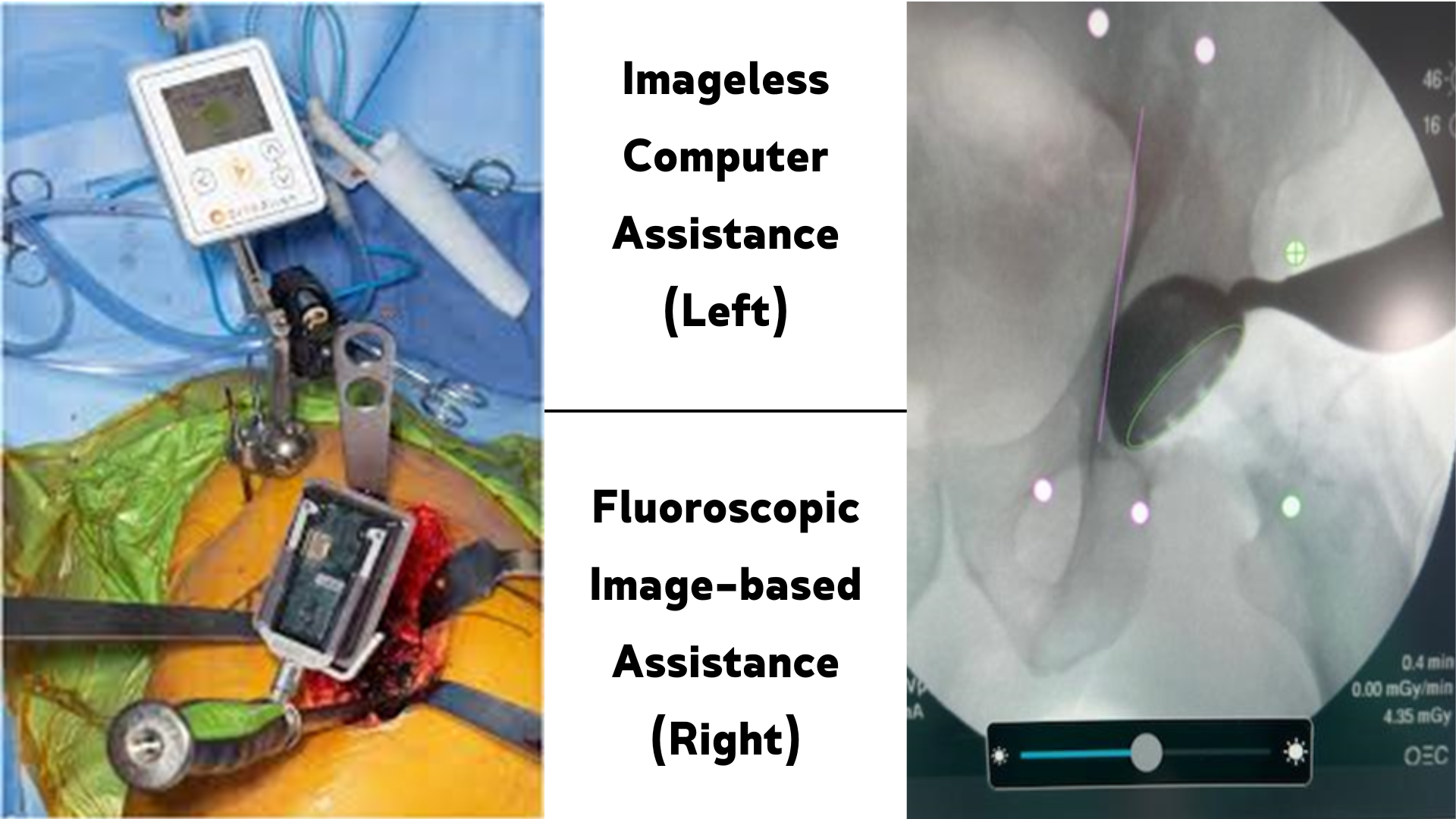
Non-robotic navigation was introduced in the 1990s. In contrast to robotic-assisted, non-robotic platforms do not perform any actions on the patient, but instead provide information to guide the surgeon. Sensors are used to track the 3-D position of the bones. There are 2 types of non-robotic navigation: 1) imageless, non-robotic and 2) image-based non-robotic. Imageless, non-robotic navigation does not require preoperative CT or intraoperative Xray (fluoroscopy) and relies solely on anatomic landmark registration in surgery to create a 3-dimension model. Image-based, non-robotic navigation requires a preoperative CT/MRI or relies on fluoroscopy. Similar to imageless, intraoperatively, anatomic landmarks are registered, usually via pin placement, to the 3-D model. With fluoroscopic navigation, conversely, anatomic landmarks are registered on the xray only; thus, no extra pins or screws are placed in surgery. Similar to other platforms, image-based leads to highly accurate implant positioning. However, compared to imageless, it is associated with increased cost from preoperative imaging and/or radiation exposure from preoperative imaging or intraoperative fluoroscopic imaging.
Computer-assistance in THR has been increasing, although it is not as widespread as usage in knee replacement surgery. From 2005 to 2018, utilization of computer assistance increased from 0.1% to 1.9%. Robot-assisted THR increased from <0.1% to 2.1% from 2008 to 2018 (3) Compared to conventional techniques, computer and robotic assisted THR results in more accurate and precise implant positioning. Additionally, recent advancements in computer-assisted platforms have been able incorporate patient-specific factors such as spinal stiffness (ie lumbar fusion), a major contributor to instability.
Non-robotic CA-THR, in comparison to robotic-assisted THR, is much less expensive for the surgical facility since robots require a significant capital investment. Also, non-robotic CA-THR requires less operative time than robotic since there are fewer disruptions to conventional surgeon workflow. Although implant positioning is improved with technology assistance, most studies have shown minimal clinical improvement. However, there has been recent literature suggesting a reduced rate of revision for dislocation (Agarwal et al 2021, JBJS), but this is far from conclusive.
After CA-THR, the recovery protocol is identical to conventional THR. Patients can place full weight on the operative extremity. A walker is typically used to ambulate for 2 to 4 weeks. Physical therapy is often prescribed, but this is based on surgeon and patient preference. Follow-up clinic appointments are important to monitor wound healing and functional recovery. Patients should remain in close contact with the physician’s team and notify them immediately with any questions or concerns. Typical return to near full function is about 6-12 weeks, but each patient’s recovery is different.
Postoperatively, hip precautions may be advised by the surgeon depending on their preference. These precautions are intended to avoid certain high-risk positions and are entirely dependent on the surgical approach. After anterior approach surgery, patients may be advised to avoid extreme hip extension and external rotation. After posterior approach surgery, extreme internal rotation and hip flexion are to be avoided. If a lateral approach is utilized, hip precautions are usually not placed.
If you or someone you know is interested in learning more about becoming a candidate for a computer-assisted total hip replacement, please click on my profile below to schedule an appointment with myself. The orthopedic specialists at Rothman are here to support you every step of the way on your journey back to specializing in what you love.
References
- Nho SJ, Kymes SM, Callaghan JJ, Felson DT. The burden of hip osteoarthritis in the United States: epidemiologic and economic considerations. J Am Acad Orthop Surg. 2013;21 Suppl 1:S1-6. doi: 10.5435/JAAOS-21-07-S1. PMID: 23818185.
- Sloan M, Premkumar A, Sheth NP. Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018 Sep 5;100(17):1455-1460. doi: 10.2106/JBJS.17.01617. PMID: 30180053.).
- Korber S, Antonios JK, Sivasundaram L, Mayfield CK, Kang HP, Chung BC, Oakes DA, Heckmann ND. Utilization of technology-assisted total hip arthroplasty in the United States from 2005 to 2018. Arthroplast Today. 2021 Oct 29;12:36-44. doi: 10.1016/j.artd.2021.08.020. PMID: 34761092; PMCID: PMC8567325.
- Agarwal S, Eckhard L, Walter WL, Peng A, Hatton A, Donnelly B, de Steiger R. The Use of Computer Navigation in Total Hip Arthroplasty Is Associated with a Reduced Rate of Revision for Dislocation: A Study of 6,912 Navigated THA Procedures from the Australian Orthopaedic Association National Joint Replacement Registry. J Bone Joint Surg Am. 2021 Oct 20;103(20):1900-1905. doi: 10.2106/JBJS.20.00950. PMID: 34143758.
- Combined Anteversion Technique for Total Hip Arthroplasty With Handheld Accelerometer-Based Navigation System Diego Alarcon Perico, MD, Christopher N. Warne, MD, Sheng-Hsun Lee, MD, Heather J. Roberts, MD, Rafael J. Sierra, MD *]]




