Knee
Rothman Orthopaedics’ Joint Replacement Program is one of the nation’s top joint replacement centers, performing more than 17,000 joint surgeries annually.
Why Rothman?
Rothman Orthopaedic Institute’s specialists offer a range of approaches, starting with conservative, non-surgical treatments such as medications, injections, and other therapies that can relieve most pain. More complicated conditions also can be addressed with minimally invasive surgery, if appropriate.
Our Joint Replacement Program gives people back pain-free mobility. With thousands of surgeries each year, we have one of the nation’s top programs for this life-changing procedure Our surgeons are extensively trained and all gain superior knowledge, skills, and expertise in their chosen subspecialty through rigorous Fellowship training programs.
The Rothman Cartilage Restoration Institute offers a new option beyond a total joint replacement. Patients who suffer with pain due to arthritis and cartilage damage can have their knees repaired through realignment surgery, ligament reconstruction, and cartilage restoration. Our specialists lead the way in this emerging field with innovative approaches so patients now and in the future can walk, run, and move again without debilitating pain.
- Our specialists are board-certified, fellowship-trained and have many years of extensive experience. Some have been team physicians for area professional sports teams.
- Rothman specialists regularly publish research in prestigious medical journals and lecture worldwide to share their vast knowledge with the next generation of orthopedic specialists.
Our nationally recognized orthopedic team has consistently ranked among the best in the Delaware Valley by US News & World Report.
-
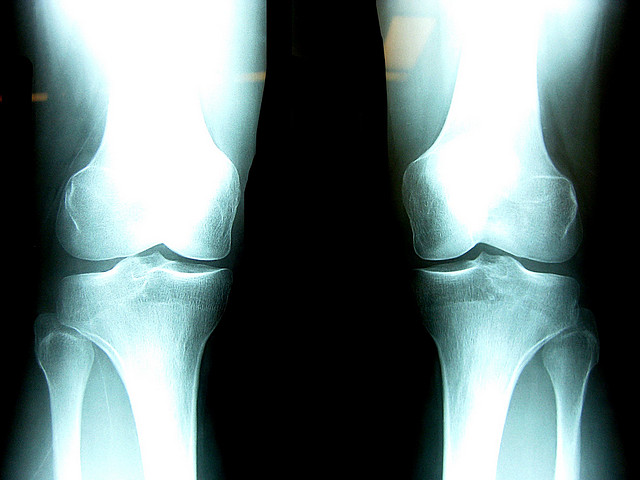
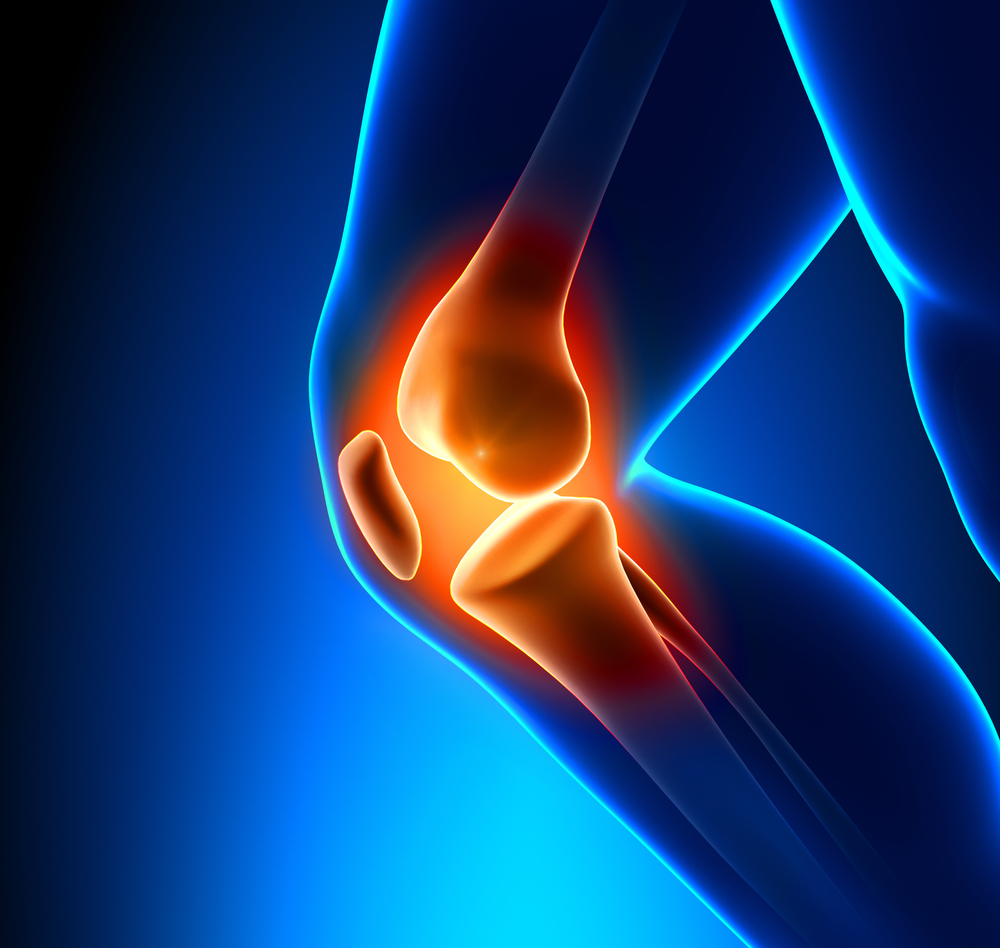
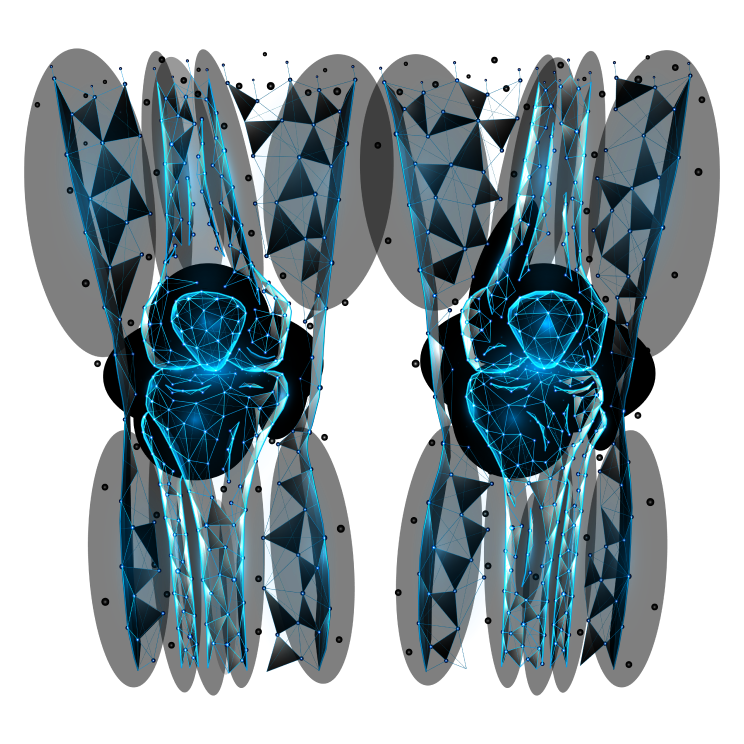
How does the knee work?
The knee joint functions like a hinge at the junction of the two largest bones: the thigh bone (femur) and the shin bone (tibia).
The knee normally bends 180 degrees in one direction — from front to back. The bones, tendons, ligaments and muscles around the knee interact to let us bend our legs to stand, walk, run, jump, sit, kick, dance, and much more.
The knee joint functions like a hinge at the junction of the two largest bones: the thigh bone (femur) and
Read More
-
What are the parts of the knee?
The two knobby ends of the femur (thigh bone) fit into round depressions in the top of the tibia (shinbone). A semi-circle of fibrocartilage called a meniscus cushions and lubricates the bone ends where they meet and acts as a shock absorber. The medial meniscus is on the inner side of the knee joint and the lateral meniscus is on the outer side.
The two knobby ends of the femur (thigh bone) fit into round depressions in the top of the tibia (shinbone). A semi-circle of
Read More
-
What are the parts of the knee? (Cont.)
The kneecap (patella) bone floats in front of the knee, protecting the joint and connecting the muscles of the front of the thigh to the tibia in the lower leg. Although not part of the joint itself, the second lower leg bone (fibula) helps support the tibia and allows the knee to rotate slightly.
The kneecap (patella) bone floats in front of the knee, protecting the joint and connecting the muscles of the front of the thigh
Read More
-
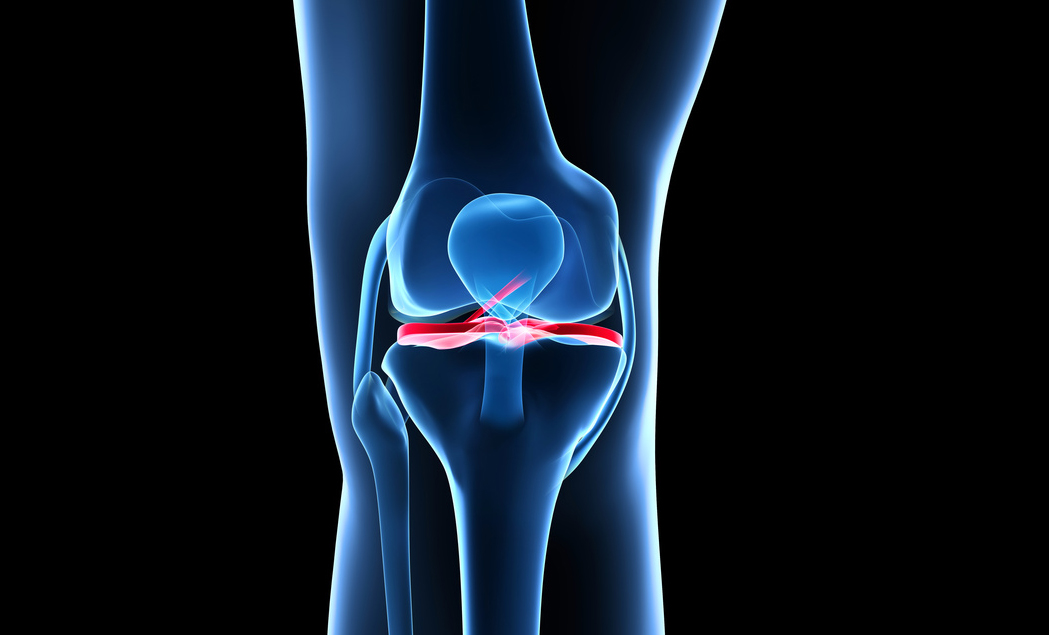
What are the parts of the knee? (Cont.)
The entire knee joint is stabilized and held in place by a network of fibrous ligaments that protect it from bending backward (called hyperextension).
The four main stabilizing ligaments are:
- Anterior cruciate ligament (ACL)
- Posterior cruciate ligament (PCL)
- Medial collateral ligament (MCL)
- Lateral collateral ligament (LCL)
Tendons connect the joint to the upper and lower leg muscles.
The entire knee joint is stabilized and held in place by a network of fibrous ligaments that protect it from bending backward
Read More
-
Why do knee problems happen?
As a weight-bearing joint, the most common knee problems involve inflammation and pain caused by arthritis and tendonitis. Overuse and pounding motions like running and jumping can wear away or damage cartilage where the joint’s bones rub together.
Accidental falls and twisting injuries can fracture the joint bones and tear ligaments, tendons, and the meniscal cushions.
As a weight-bearing joint, the most common knee problems involve inflammation and pain caused by arthritis and tendonitis. Overuse and
Read More
-
Common Conditions
- Anterior Cruciate Ligament (ACL) Injury
- Bony Stress Reactions/Stress Fractures
- Cartilage Injuries
- Chondromalacia patella (Runner’s Knee)
- Knee Arthritis
- Lateral Collateral Ligament Injury (LCL) Injury
- Medial Collateral Ligament (MCL) Injury
- Meniscal Deficiency
- Meniscal Tear
- Patellar Subluxation - Dislocation (Unstable Kneecap)
- Patellar Tendonitis
- Patellofemoral Pain Syndrome
- Posterior Cruciate Ligament Injury (PCL) Injury
- Running/Pivoting/Jumping Sports Injuries
-
Health Tips
- Lose weight. You’ll put less pressure on your knees and reduce pain.
- Strengthen leg and thigh muscles. Low-impact exercises like walking and strength training can preserve the cartilage on the ends of your leg bones. Stretching improves range of motion.
- Stay active every day. Moving around reduces joint stiffness and helps keep a healthy muscle mass.
- Take anti-inflammatory medications to reduce pain and swelling.
- See a specialist if pain or swelling persist.
- View All
- Abington Hospital - Jefferson Health
- Abington Lansdale Hospital - Jefferson Health
- AdventHealth - Kissimmee, FL
- AdventHealth Altamonte Springs
- AdventHealth East Orlando
- AdventHealth Heart of Florida
- AdventHealth Orlando
- AdventHealth Surgery Center Innovation Tower
- AdventHealth Training Center - Orlando, FL
- AdventHealth Winter Garden
- AdventHealth Winter Park
- AtlantiCare - Center for Orthopaedic Surgery
- AtlantiCare Regional Medical Center (Mainland Campus)
- Bensalem, PA
- Bordentown, NJ
- Bryn Mawr Hospital
- Bryn Mawr Hospital Orthopaedic Surgery Center
- Bryn Mawr, PA
- Cape May Court House, NJ
- Capital Health Medical Center, Hopewell
- Center City Philadelphia
- Chalfont, PA
- Davenport, FL
- Doylestown Ambulatory Surgical Center
- Doylestown, PA
- Egg Harbor Township, NJ
- Glen Mills, PA
- Hamilton, NJ
- Innovation Tower, Orlando, FL
- Jefferson Bucks Hospital
- Jefferson Orthopedics Bucks County
- Jefferson Surgery Center - Cherry Hill
- Jefferson Washington Township Hospital
- King of Prussia, PA
- Lake Mary, FL
- Lake Nona, FL
- Lankenau Hospital
- Limerick, PA
- Malvern, PA
- Manahawkin, NJ
- Marlton, NJ
- Media, PA
- New Jersey Surgery Center
- Newtown, PA
- Northeast Philadelphia
- Paoli Hospital
- Pennington, NJ
- Physicians Care Surgery Center
- Physicians Care Surgical Hospital
- Princeton, NJ
- Riddle Memorial Hospital
- Riverview Surgical Center
- Robert Wood Johnson University Hospital, Hamilton
- Rothman Orthopaedic Specialty Hospital
- South Philadelphia
- Thomas Jefferson University Hospital
- Washington Township, NJ
- Willow Grove, PA
- Winter Garden, FL
- Winter Park, FL
- Wynnewood, PA
- View All
- Female
- Male
- View All
- Non-Surgeons
- Surgeons
Sort
-
- FL
-
- PA
-
- FL
-
- PA
-
- NJ
- PA
-
- PA
-
- PA
-
- NJ
- PA
-
- PA
-
- PA
-
- PA
-
- NJ
- PA
-
- PA
-
- PA
-
- NJ
-
- FL
-
- FL
-
- NJ
-
- NJ
-
- NJ
- PA
-
- PA
-
- PA
-
- PA
-
- PA
-
- FL