Back and Hip Pain in Athletes (Part 2): Symptoms, Evaluation and Treatment Options
In part 1, we discussed (link here) pain in this region in active individuals can be challenging to diagnose and treat. The bottom line is a careful and detailed history and evaluation by a specialist with spine and musculoskeletal expertise. This is absolutely crucial to avoid delay in diagnosis and development of a chronic pain condition that is refractory to the traditional treatment approaches.
What are my symptoms if these muscles are involved and what kind of specialist should I see?
Depending on the origin of your pain, you may experience low back pain, buttock pain, coccyx pain, sacroiliac joint pain, hip or groin pain, pain with sitting or pain with exercise. Since these muscles also help the pelvic organs, it is not uncommon for patients to experience symptoms related to bladder or bowel such as urinary frequency, urgency, pain with urination, constipation, urinary or bowel incontinence, pelvic pain or rectal pain. If your causes for your symptoms have been checked by an urologist and/or a gynecologist and if it is not related to your bladder, bowel or gynecological problem, an orthopedic or spine specialist with expertise in the hip, spine and pelvic region would be the person you would need to see.
Can the pain and the symptoms be nerve related?
Pelvic floor also has a complex neuromuscular anatomy and irritation or entrapment of these nerves within the musculature can result in nerve pain called neuropathic pain. A common nerve that can be irritated with activities such as biking, prolonged sitting and playing tennis is pudendal nerve. Pudendal nerve pain or pudendal neuralgia can be very disabling but is a definitely treatable condition if proper education, lifestyle changes and exercises are adopted with persistence.
How do we evaluate our patients with spine, hip and pelvic pain?
Evaluation of this problem starts with an extensive history with focus on when the pain started, co-existent symptoms related to pelvic organs, prior treatments, trauma, surgery, childbirth etc. and whether brain hypersensitivity has already occurred is important to identify the barriers for progress. We do a comprehensive spine, hip, pelvis and lower extremity evaluation to identify the pain generator and additional impairments. This includes musculoskeletal and neurological exam and pelvic floor exam that should be performed by an appropriately trained specialist capable for incorporating all these systems in their examination or able to work with a multidisciplinary team. Individualized treatment plan is important to establish clear goals for each individual “as one size does not fit all”
What are the treatment options?
A specific exercise regimen or physical therapy prescription for the individual patient describing the biomechanical and neurological impairments is necessary that guides other caregivers like physical therapists to deliver appropriate treatment without wasting time.
In addition to exercises, sometimes multimodal approach is considered that includes appropriate medication prescription such as analgesics, anti-inflammatory medications, muscle relaxants, anti-anxiety medications and neuropathic medications as appropriate. In general, opioid medications are not preferred first line treatment as there are no clear long-term benefits.
For patients who fail to respond to initial conservative measures or if pain is severely limiting their progress with therapy, X-Ray guided injections are considered such as pudendal nerve blocks, sympathetic blocks, nerve plexus blocks, epidural injections, sacroiliac joint injections, pelvic floor muscle trigger point injections and neuromodulation. Surgical considerations will depend on the underlying condition and appropriate patient selection.
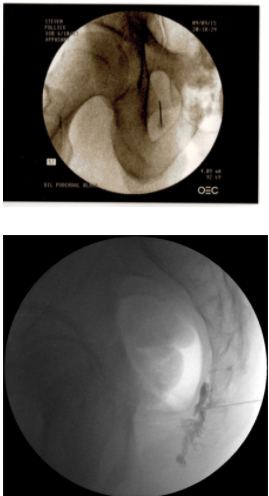
Fig 6: X-ray guided pelvic injections
We emphasize the importance of healthy lifestyle changes such as healthy voiding and bowel function, proper posture, appropriate stretching and exercise modifications, nutrition, sleep and mindfulness to be incorporated for long term success.
Can I return to the activity that I enjoy?
Absolutely! You never have to stop enjoying the things that you love. Proper evaluation and a guided treatment plan by appropriately trained specialist are your first step towards your road to recovery. We can help you reach your individual fitness goals.




