Bringing Dual Mobility Total Joint Replacement for Thumb Basal Joint Arthritis to the United States
Introduction
Thumb basal joint arthritis (a.k.a. CMC-1 joint or carpo-metacarpal joint) is the second most common form of osteoarthritis occurring in the hand, but it is the most common form of arthritis that undergoes surgery. The CMC-1 joint is comprised of the metacarpal and trapezium bones that meet like two saddle shapes where the thumb ray meets the wrist. The unique shape gives the thumb a wide range of mobility to acquire an object, and stability to keep an object. Because of the stresses placed across the joint over a lifetime, cartilage wears away in a similar fashion to that of knees and hips. The typical individual with symptoms is aged 50-75 years who notes a gradual increase in pain where the thumb meets the wrist. Pain with activities like twisting a jar top or pinching a key are common complaints; some patients even admit to leaving all their jar tops half-open in their refrigerator!
When meeting with your doctor, the first recommendations usually start with awareness of avoiding the aggravating movements (heavy pinching), bracing, or injections with corticosteroids. However, if all non-surgical measures have failed and the problem persists, then surgical options could be discussed.
The most common method for surgically treating CMC-1 arthritis in the United States is a “resection arthroplasty.” These procedures take some variations, but ancestrally date back to 1949 when the first resection of the trapezium bone was recorded. The idea comes from the premise that with osteoarthritis, the bones lost the space that was formed by the cartilage and the bones scuff against one another. So, by removing the smaller bone, the surgeon creates a space that fills in with scar tissue. In other words, instead of grinding bone on bone, the thumb is now bone on a softer scar pad. These procedures work well to reduce pain and are still the most common method of surgery, but drawbacks include thumb shortening, weakness in pinch, issues with stability, and crookedness of the MP joint (the next joint where the thumb meets the hand).
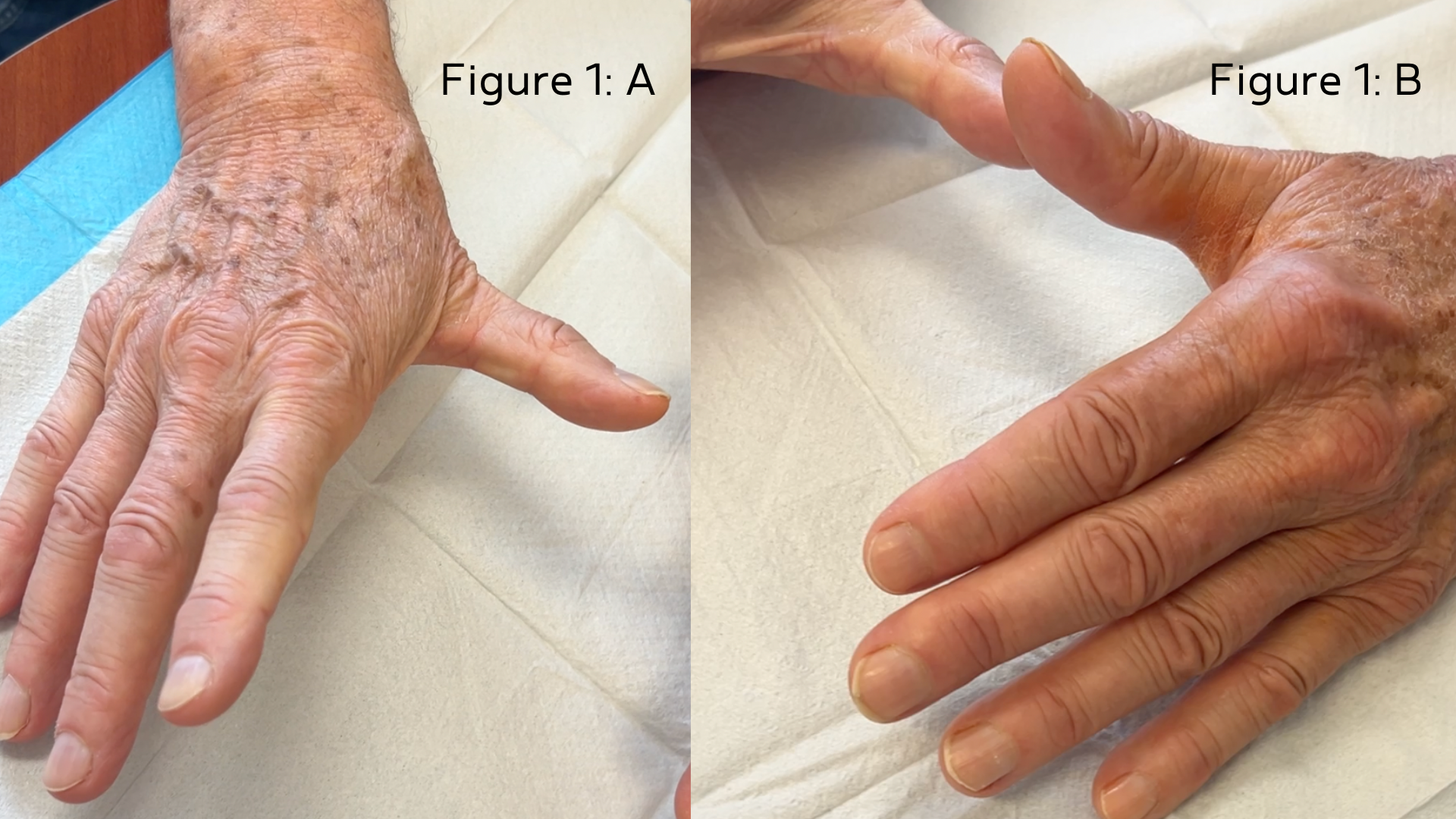
(Figure 1: A. Classic “Z” deformity on the right thumb (left panel) treated with resection technique. B. Restoration of thumb length and balance with implant procedure of the left thumb (right panel).
What Is Dual Mobility Total Joint Replacement?
The first joint replacements for the CMC-1 joint had problems with loosening and dislocation. These were largely abandoned by the U.S. surgeons but continued to evolve in Europe. At the international hand surgery meeting a few years ago, European surgeons and American surgeons hotly debated this topic whereby the European surgeons had shown strong evidence for improved design and technique, with high quality data showing not only safety, but also advantages over trapezium resection such as improved strength, more natural range of motion, and deformity correction.
The current design is very similar to a hip replacement. The arthritic surfaces are replaced with a press-fit titanium ball and cup design.

(Figure 2: Dual mobility ball and socket design of the “Touch” prosthesis)
The dual mobility design allows motion between the plastic ball and the cup, as well as between the metal head and the plastic ball. This improves the “flexibility” of the implant and reduces dislocations.
In Europe, the CMC-1 dual mobility implant is new, but two clinical trials have reported 2-year and 5-year outcomes showing survival of approximately 100% and 95% respectively. When compared to traditional techniques, trials have shown superior strength, mobility, deformity correction, and recovery time.
Rothman’s Breakthrough Moment
In July of 2025, the FDA had recently approved dual mobility arthroplasty in the United States, with Dr. Richard Tosti of Rothman Orthopaedics successfully performing the first few cases in the United States at Rothman’s Physician Care Surgical Hospital in Limerick, PA. Dr. Tosti spent this past winter learning from thought leaders in Belgium and France in order to bring the technology to the Philadelphia region. Currently, the implant is only being released to surgeons with the requisite training. “I think it shows honorable ethics on the part of the company,” Tosti said. “They want good outcomes in experienced hands, and they want to see if we can reproduce the success seen in Europe.”
Why This Matters for Patients
European data suggests that patients return to work faster, have less pain, more natural motion and appearance, and better strength with the implant arthroplasty, compared to older resection techniques.
As of the publication of this article, this surgery is only accessible in the United States through Dr. Tosti and Rothman Orthopaedics. In 2025, only about 15 academic hand surgeons across the United States have completed formal training – Dr. Tosti being the only one in the greater Philadelphia region.
Meet the Surgeon
Dr. Tosti is an orthopedic trained upper extremity surgeon who holds a double rank of Associate Professor at Thomas Jefferson University College of Medicine and Drexel University School of Medicine. He also serves as a program director for the hand and microsurgery fellowship training program at Thomas Jefferson University. He is a licensed ringside medicine doctor for professional boxing and MMA. He has published multiple scientific articles and has spoken nationally on the topic of CMC-1 arthritis and has been the recipient of several national research awards and local top doctor accolades. Dr. Tosti sees patients at Rothman’s Limerick and Bryn Mawr Offices. To schedule a consultation with him, visit his profile or our appointments page today.




