Detailed Exploration of Radiofrequency Ablation
What is medial branch radiofrequency ablation?
A medial branch radiofrequency ablation procedure (also known as radiofrequency neurotomy or a rhizotomy) is a non-surgical, outpatient, minimally invasive pain management procedure that can greatly improve axial back pain by targeting the nerve supply of painful arthritic spinal joints. The radiofrequency ablation procedure uses advanced machinery that generates radio waves to heat the tip of specialized needles to cause a thermal lesion at the site of small nerve branches called medial branches. These medial branches supply the facet joints in the spine and ablating them interrupts their ability to transmit a signal from painful arthritic spinal joints to the spinal cord and brain. Each arthritic facet joint in the spine is covered by two medial branches that can be targeted using image guided needle placement.
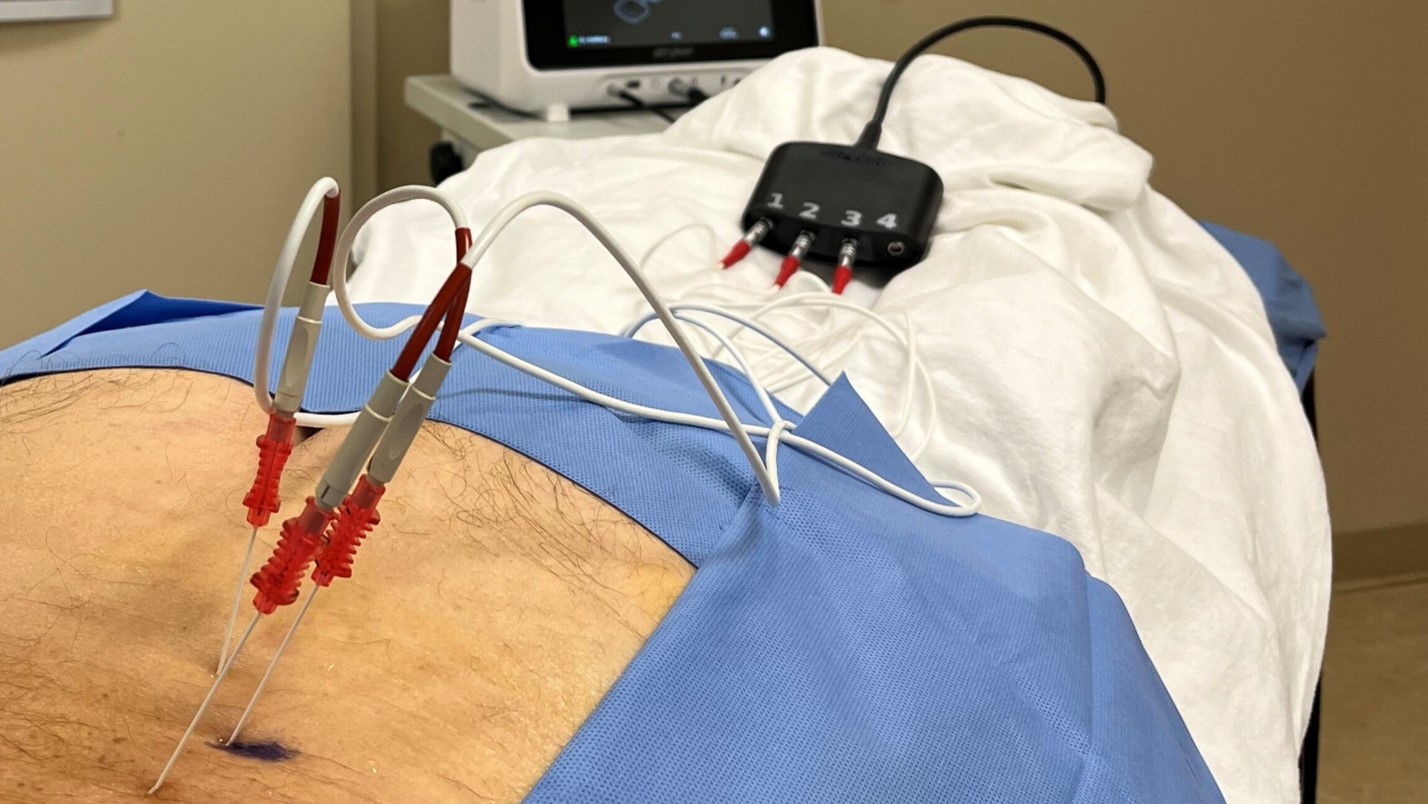
Example of a Radiofrequency Ablation being performed
Which patients would benefit from radiofrequency ablation?
Candidates for this procedure are selected based on having certain findings on their physical examination and history such as extension based back pain often worse with twisting, inability to stand up straight due to back pain or prolonged back pain in the morning. These symptoms are then correlated with spinal imaging studies which show facet joint arthritic changes. The radiofrequency ablation procedure is typically offered to patients whose back pain has not responded to other forms of treatment including physical therapy, home exercises and anti-inflammatory medication. The ablation procedure targets back and not leg pain symptoms.
Prior to proceeding to the radiofrequency ablation procedure, the first step is to block the medial branches using an anesthetic medication injected through needles under fluoroscopy (live X-ray guidance). This initial step is called a medial branch block and is often done twice prior to selecting good candidates for medial branch radiofrequency ablation procedure. If the arthritic facet joints are the true dominant source of the patient’s back pain, then the patient would note profound short-term pain relief in the hours following the block procedures (often 80% or greater relief). Improved functionality is often associated with this pain relief as well. If the patient notes only mild or moderate pain relief following the branch blocks then they are not an ideal candidate for a spinal radiofrequency ablation procedure and the spinel physician will investigate for other possible sources of their spinal pain, including disc pathology, muscular pain, or spinal stenosis.
Other conditions treated with radiofrequency ablation
Common spinal conditions targeted with medial branch radiofrequency ablation include arthritic low back, midback or neck pain as well as sacroiliac joint pain (the latter by targeting lateral branches). More recently this technology has expanded to target nerve supply that also supplies large peripheral joints, such as the knee, hip, and shoulder. You may also be aware of other non-spinal applications of ablation technology such as targeting cardiac tissue, peripheral veins, and tumor conditions.
How exactly is a radiofrequency ablation procedure performed?
The spinal radiofrequency ablation procedure is performed with sterile technique in a procedure room setting using fluoroscopy both for guidance of needle placement as well as to safely visualize the spinal anatomy. A ground electrode pad is placed on the patient for the procedure as part of our safety protocols.
The medial branch radiofrequency ablation procedure uses local anesthetic medication to numb the skin prior to the placement of each needle. Patients are generally awake for the procedure as the doctor and patient interact during the procedure. Just prior to ablating the medial branch nerves, the doctor performs sensory and muscle response testing of the medial branches to confirm placement and asks the patient for feedback on the symptoms that they feel during these testing stages as well as during the ablation phase. The doctor will verify with the patient that no pain or numbness symptoms refer past the low back and buttocks region further down the leg as we are avoiding the exiting larger spinal nerves. Generally, the lesioning phase of the procedure is very well tolerated with minimal pain noted. The procedure can take anywhere from 10 to 25 minutes depending on the number of branches targeted. Generally, we target anywhere from two branches (if there is only one facet joint targeted) or up to six medial branches at a time (if two facet joints are targeted on each side).
Pre-procedure instructions
The patient should prepare for the procedure by arranging for transportation from a family member or friend, and by only eating a light meal that morning. Prior to the procedure we can discuss which medications would need to be continued or stopped prior to the procedure. We would also discuss any need for an anxiolytic medication that you may wish to take pre-procedure for relaxation.
As with any procedure that passes through the skin, there is a very small risk of significant bleeding or infection, and every precaution is taken to avoid these. There is also a small chance of some skin numbness in the region that was ablated that would improve with time.
Post-procedure care and outcomes
After the ablation, notable relief of back pain can start anywhere between one and three weeks. The first week post procedure there can be some increased muscle soreness and pain. The patient and doctor will discuss ahead of the procedure any medication that the patient can take for this pain. Ice can also be applied intermittently to the procedure sites during the first day upon returning home. Usually, the most profound pain relief starts to take effect between weeks two and three post procedure. The length of the pain relief can last anywhere from 6 to 18 months. If the procedure provides extended relief for at least 6 months and the same back pain returns, we can simply repeat the radiofrequency ablation at that time targeting the nerve branches that regrew.
Extremity symptoms such as nerve pain, numbness, tingling, and weakness are not expected after the radiofrequency ablation procedure as the spinal nerve roots that exit the spine and radiates down the legs or arms are not being targeted. The doctor will ensure that they are not near the spinal nerve roots based on the visualization of needle placement under fluoroscopy as well as based on the patient’s symptom responses during the testing and ablation phases.
About 70% of patients will note good to excellent pain relief of their arthritic spinal pain with the radiofrequency ablation procedure over time. If the ablation procedure still fails to provide the desired pain relief, then the spine physician will help the patient identify other sources of spinal pain, such as disc degeneration, disc herniation, spinal stenosis, or muscular pain.




