Hip Replacement vs Hip Resurfacing
What is a Total Hip Replacement?
Total hip replacement is a procedure utilized to remove arthritic changes in the ball and socket joint of the hip. When the hip has lost the cartilage, which is the smooth surface at the edge of the bone, it becomes painful and can cause loss of mobility and function. Joint replacement is an option to alleviate the pain and improve function.
How is Total Hip Replacement different from Hip Resurfacing?
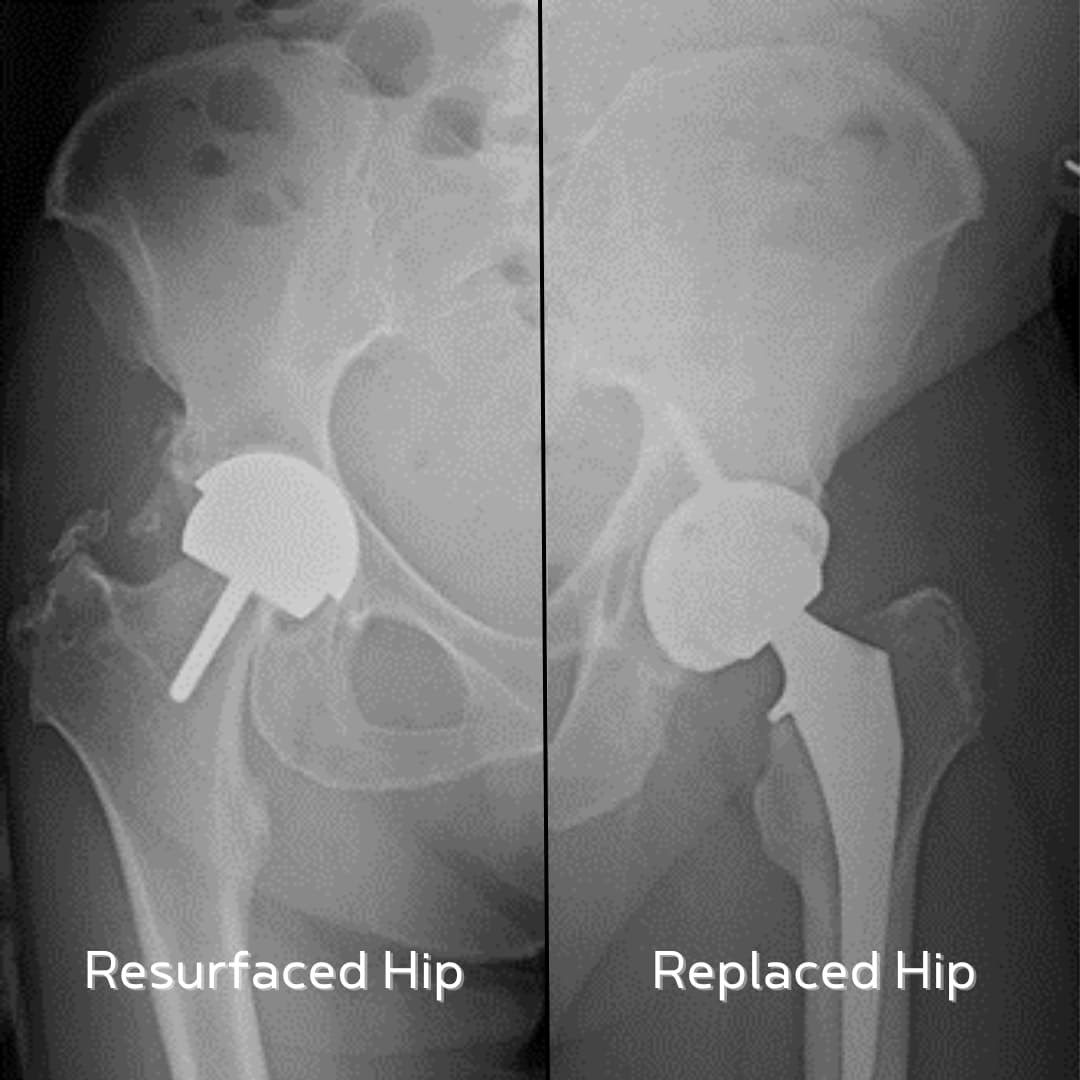
Hip replacement and hip resurfacing are very similar in concept as both aim to remove the worn out surface on both the femoral (ball) and acetabular (socket) side of the joint. The two operations differ in that a resurfacing attempts to persevere the area of the ball and place a cap over top of the native area.
In a total hip replacement the area of worn out bone is removed and the replacement is placed inside of the bone, as compared to a resurfacing on top of the bone. Both procedures from the socket side are the same.
Is preserving my bone better?
Hip resurfacing was developed with the concept of preserving the native femoral head (ball) in order to place as large of a replacement head as possible. The desire for doing so was two-fold. The first benefit was to decrease the risk for dislocation and the second was to provide an alternative bearing surface (metal on metal) compared to traditional hip replacement, which was metal on polyethylene (surgical plastic).
Historically, the concern for dislocation was elevated as the hip capsule was not surgically repaired; originally, the area of bone providing the attachment for the hip stabilizers was detached (osteotomy) during surgery. Today, we have continued to develop techniques to minimize the risk for dislocation, including the repair of the capsule, avoiding the osteotomy, the addition of fluoroscopic assisted or computer navigated surgery and dual mobility components. There has also been a large increase in the knowledge base surrounding the spinopelvic relationship, which has helped to reduce the risk for dislocation even further.
The concern of polyethylene (surgical plastic acting as the cartilage) wearing out had become a true concern. After 10 years, the insert was wearing and requiring a second surgery in many cases. Today, we have moved on from the 1st generation polyethylene inserts, and now utilize the third generation of the inserts, which has incredibly low wear rates. The current technology has been utilized for around 9 years to date, and has produced effective results, which may lead to much longer lifespans of the replacements.
Does Hip Resurfacing make it better for me if I am younger?
While the concept of bone preservation is one that can be quite attractive, our current technology allows for the replacement head and polyethylene liner (artificial cartilage) to be modular. This allows the implant surfaces that are attached to the bone to be maintained at the time of a second surgery, if required. If a hip resurfacing required a revision (second surgery) to a total hip replacement, it would require bone removal to place the new stem and ball, making the concept of bone preserving one of less practicality.
What if the Total Hip Replacement needs to be revised?
If the femoral stem needs to be placed after total hip replacement it would require a longer metal replacement. This would require more bone involvement, meaning a conversion from a hip resurfacing to a total hip replacement.
Hip Resurfacing History
Hip resurfacing in the 1990s attempted to solve the problem of polyethylene wear and dislocation by implementing large diameter metallic femoral heads (ball) on a metallic liner (socket). The wear rates of the metal on metal articulation was extremely low, however, the metallic debris created was not tolerated well by the body. The metal produces an adverse local tissue reaction resulting in tissue destruction, pain and implant failure.
The large metallic heads were also not suitable for female patients and patients with smaller femoral head (ball) sizes as they were at risk for fracture (breaking) of the femoral neck (the bone they were attempting to preserve). The complications associated with the implants lead to all but one implant for hip resurfacing being removed from the market.
Candidates for Total Hip Replacement
Candidates for total hip replacement are not exclusive of age or gender. It is not exclusive for diagnosis of underlying arthritic process (osteoarthritic, rheumatoid arthritis, avascular necrosis, etc.) Candidates need to be in an optimized medical condition, including but not limited to, their cardiac or pulmonary illnesses, diabetes and weight.
Candidates for Hip Resurfacing
When looking at who should be considered for hip resurfacing, acknowledging the risk for failure as stated above, success was most often found in males less than 60, with osteoarthritis and a femoral head size greater than or equal to 48mm. Most surgeons would not recommend resurfacing in females of child-bearing years, as the metallic debris can cross the placental barrier.
Recovery after Total Hip Replacement and Hip Resurfacing
The procedure for hip replacement and resurfacing is typically between 60 to 90 minutes. The operation is performed in both the outpatient setting (home same day), as well as with overnight stays and a return home the following day. The decision on length of stay is based on medical condition, age, motivation and home support.
The first 6 weeks following surgery are spent allowing the body to recover. You are up walking day of surgery and wean from any assistive device (cane or walker) as tolerated. For some individuals this could be as soon as a few days, and for others, could be a few weeks. Most individuals note a significant improvement in pain shortly after surgery, however, it takes 3 to 4 months for the majority of the healing process to occur. The vast majority of my patients do not require any formal physical therapy after hip replacement.
Complications after Hip Surgery
-
Infection: Infection is a serious risk of any surgery, including hip resurfacing or replacement surgery. The risk of infection is typically low, but it can be serious if it does occur. Infection can lead to pain, swelling, redness, and warmth around the incision site. It can also lead to loosening of the implant and the need for further surgery.
-
Bleeding: Bleeding is another risk of any surgery, including hip resurfacing and replacement surgery. The risk of bleeding is typically low, but it can be serious if it does occur. Bleeding can lead to a need for blood transfusion.
-
Nerve damage: Nerve damage is a rare but serious risk of hip resurfacing and replacement surgery. Nerve damage can cause numbness, weakness, and pain in the leg and foot. It can also make it difficult to move the leg.
-
Blood clots: Blood clots can form in the veins of the arm or leg after surgery. These blood clots can travel to the lungs, heart, or brain. Blood clots are a serious risk, but the risk can be decreased with early, frequent walking and with medication.
-
Implant failure: The implants used in hip resurfacing and replacement surgery can sometimes fail. This can lead to pain, instability, and the need for further surgery.
-
Dislocation: The hip joint can sometimes dislocate after hip resurfacing and replacement surgery. The risk can be slightly higher with hip replacement. Dislocation can be painful and can require surgery to repair.
-
Need for revision surgery: In some cases, it may be necessary to have revision surgery after hip resurfacing or replacement surgery. Revision surgery is surgery to replace or repair the implants that were used in the initial surgery.
What are the long-term outcomes after Hip Replacement?
After hip replacement there is a 90-95% good to excellent outcomes reported by both patients and physicians.
What are the long-term outcomes after Hip Resurfacing?
After hip resurfacing the outcomes have significant differences based on implants utilized with the Birmingham hip having a 10.8% revision rate compared to the Depuy ASR having a 35.2% revision rate. There is new technology attempting to look at a metal on polyethylene hip resurfacing which has not been adopted into the mainstream in the United States.
When to decide on Hip Surgery and How?
The decision to move forward with hip surgery be it a resurfacing or a replacement is truly an individualized process. When someone has come to the point of making compromises and sacrifices in their daily lives because of the pain and limitations their hips give them, they will be ready for surgery. The decision of choosing between a hip resurfacing and replacement is one that can be discussed between you and your doctor to weigh the potential risks for benefits.
Should you want to discuss your hip, please consider making an appointment today.




