The Different Types of Bunion Treatments
What are bunions?
A simple definition for a bunion is a bony bump that forms on the inside of the big toe joint. In reality, a bunion deformity is a complex deformity involving the first metatarsophalangeal joint (MPJ), the big toe (hallux), and the first metatarsal. In a patient without a bunion, the first metatarsophalangeal joint is held in a proper, straight position by the ligaments, tendons, and bony architecture associated with the joint. These structures are compromised in a patient with a bunion leading to instability of the joint and the formation of the bony bump. The bony bump is the first metatarsal head pushed against the skin as the big toe moves in the opposite direction to the smaller toes. A bunion is a common aliment among the adult population, with a prevalence over 20% in adults aged 18-65 years old. The rate increases to 35% in patients older than 65 years1.
What causes bunions?
The exact cause of the bunion deformity is not well understood but studies support that there are multiple risk factors leading to the condition. These factors include genetics, sex, age, and constricting footwear.
• Genetics - Studies have shown that 90% of patients who have a bunion deformity also have at least 1 family member who also has bunions2.
• Sex - Differences in female anatomy compared to males is likely the reason that females are 2x as likely to develop bunions. Females tend to have more flexible soft tissue that can alter the stability of the big toe joint3
• Age - As the body matures, stability of the first metatarsophalangeal joint decreases as ligaments lose tension and muscle mass decreases
• Constricting footwear - There is conflicting data on whether high heels or tight fitting shoes are a sole contributor to bunion deformities. It is more likely that non-accommodative shoe gear can accelerate the progression of an already present bunion deformity.
What are the symptoms?
• Bump on the inside of the big toe
• Redness, swelling, or pain around the big toe
• Numbness of big toe
• Limited motion of the big toe
• Calluses
Possible complications associated with bunions
A bunion deformity alters the biomechanics of the foot causing a cascade effect on nearby structures. Three common complications associated with bunions include hammertoes, metarsalagia, and bursitis
• Hammertoes - With every action there is an equal and opposite reaction. This statement holds true in the foot as well. As the big toe moves towards the lesser toes, it is pulled underneath the second toe. This action forces the second toe in an elevated position and can cause a hammertoe contraction.
• Metatarsalgia - In a normal foot, the first metatarsal bears a majority of the body’s weight when walking. With a bunion, the first metatarsal is no longer in a position to support the weight and the stress is passed to the ball of the foot. Patients may notice increased pain with impact activities such as running or jumping.
• Bursitis - The body forms fluid-filled sacs called bursas over bones to promote smooth motion of tendons, ligaments and the skin. A bunion creates increased stress to the bursa leading to inflammation and increased pain.
Diagnosis of Bunions

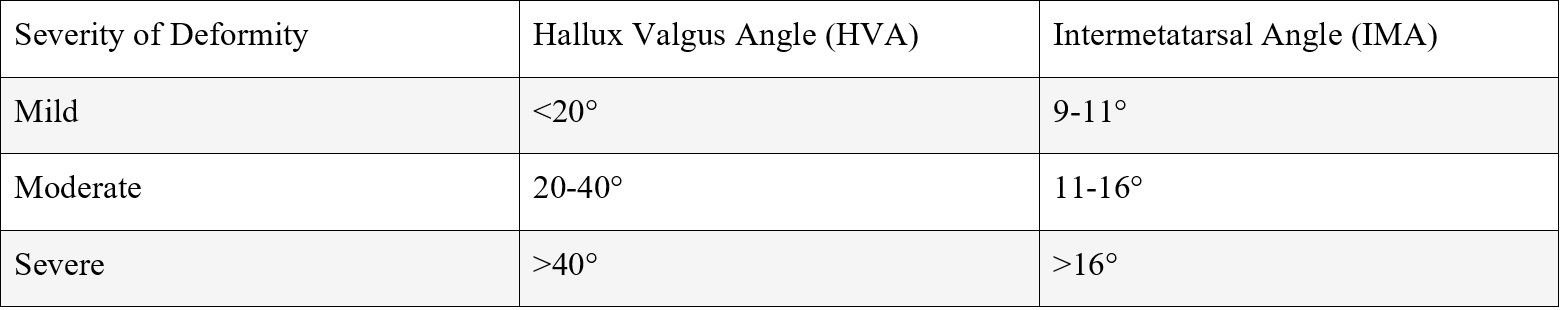
A physician will diagnosis a bunion based on the patient’s history, physical examination and radiographs. A thorough physical examination can help dictate the appropriate treatment options available for the patient. Severity of the deformity can be determined with the help of X-rays. Bunions can be classified by severity into three groups based on the measurements of the hallux valgus angle (HVA) and the first-second intermetatarsal angle (IMA). The hallux valgus angle is defined as the angle between the big toe and the first metatarsal. The intermetatarsal angle is the angle of the long axis of the first and second metatarsals4.
Conservative Bunion Treatment
• Shoe modifications - A wider shoebox allows a larger space to decrease the irritation of the bunion. Inserts with rigid arch support can also be beneficial as they improve the biomechanics of the foot. Both over-the counter, and prescription orthotics are available.
• Spacers/pads - A toe spacer between the first and second toe can help keep the big toe straight. This can help prevent pain by decreasing the prominence of the bunion as well as reduce the stress placed on the second toe by the big toe. Pads and sleeves can alleviate pain by protecting the bunion from rubbing inside of shoes.
• Ice - Applying ice to the affect foot for 15 minutes, 3-4 times a day can reduce pain.
• Anti-inflammatories - Over the counter anti-inflammatories such as ibuprofen and Tylenol can provide quick relief by reducing the amount of swelling and pain. Long term anti-inflammatory use is not recommended, always discuss with your doctor if nonsteroidal anti-inflammatories are right for you.
• Physical therapy - Physical therapy can provide symptomatic relief in bunions by strengthening the muscles of the foot. A combination of weekly physical therapy sessions and consistent toe spacer use has shown to improve symptoms.
When to get bunion surgery
Unfortunately, bunions are not curable with conservative treatment. Most bunion deformities can be managed with conservative care and patients can live their entire life without needing surgery. Surgical intervention should be considered if the bunion continues to alter day-to-day activities after conservative treatment options have been exhausted.
Types of bunion surgery
There is not a single procedure that can be used for all bunion deformities. Each patient presents with different symptoms, severity, and postoperative goals that need to be heavily considered prior to selecting a procedure. Surgical options range from simple soft tissue releases for mild deformities to fusion of joints for more severe cases. More than one procedure may even be required to correct the deformity. A thorough discussion with a Foot and Ankle provider will help lead to the best match for the patient.
Bunion Treatment Recovery
The recovery process is dependent on the severity of the bunion and the type of procedure used to correct it. Early weight-bearing may be appropriate in procedures for mild deformities but more aggressive surgeries may require an extended time of non-weight-bearing of the surgical foot. Full recovery may take weeks to months as swelling can persist after surgery.
When to see a doctor?
A bunion can be treated with home remedies, but sometimes that is not enough. You should see your foot and ankle specialist if you experience
• Continued big toe pain without relief
• Decreased range of motion of big toe joint
• Difficulty wearing certain types of shoewear
• The bunion is keeping you from living the life you want to live
At Rothman Orthopaedics, you will find a team of such specialists working together to provide patients with the best possible diagnosis, treatment, and rehabilitation.
Dr. Christopher L. Reeves is a nationally recognized, board certified Podiatric Foot & Ankle Surgeon who has been serving Central Florida since 2004. He provides comprehensive care for all ages and conditions affecting the foot and ankle and has specialized training and interest in complex reconstruction, lower extremity trauma, and total ankle replacement.
References
1. Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010;3:21
2. Coughlin MJ, Jones CP. Hallux valgus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007;28(7):759-777
3. Perera AM, Mason L, Stephens MM. The pathogenesis of hallux valgus. J Bone Joint Surg Am. 2011;93:1650-1661.
4. Smith JT, Bluman EM. Hallux valgus and hallux varus. In: Orthopaedic Knowledge Update: Foot and Ankle. 5th ed. Rosemont: American Academy of Orthopaedic Surgeons; 2014:183-191.
5. Hatch DJ, Smith B, Santrock RD. Hallux Valgus. Foot Ankle Orthop. 2019 May 7;4(2):2473011419838500. doi: 10.1177/2473011419838500. PMID: 35097321; PMCID: PMC8696753.
6. Abdalbary SA. Foot Mobilization and Exercise Program Combined with Toe Separator Improves Outcomes in Women with Moderate Hallux Valgus at 1-Year Follow-up A Randomized Clinical Trial. J Am Podiatr Med Assoc. 2018 Nov;108(6):478-486. doi: 10.7547/17-026. Epub 2018 Apr 23. PMID: 29683337




